Robot-Aided Ankle Rehabilitation In Stroke: What’s The Evidence?
Can robotics facilitate recovery of walking function after a stroke?
Our research team has pursued this question over the past two decades, investigating stroke as a model system. Nearly three of four stroke survivors have deficits that persistently impair function. In particular, hemiparetic gait is common and contributes to falls in ~70% of people within the first year. Gait deficits limit free living mobility and propagate frailty via physical and cardiovascular deconditioning. These conditions are linked to elevated risk factors for heart disease, recurrent stroke, and dementia. Gait and balance must be improved to break this vicious cycle to recover safe mobility and improve heart and brain health, which are dependent on physical activity. We advance new strategies to improve mobility and health after stroke through a series of questions posed in randomized studies.
QUESTION #1: Can walking function be improved by locomotor task practice, by what mechanisms, and within what time window after a stroke?
Stroke survivors can improve their walking function by mechanisms of neuroplasticity; activating deep subcortical networks that are located below the level of most human hemispheric strokes. Neuroanatomically, this activation encompasses the mesencephalic locomotor network, known to regulate walking in animals. The findings give stroke survivors hope to fight back against disability with locomotor task practice, even years post-stroke. Training modalities such as task-oriented exercise has been shown to reverse pre-diabetes increase fitness levels, brain blood flow, and improve cognitive function to enhance motor learning. Thus, there is a synergy of motor learning with exercise to improve neurological function, heart, and brain health. However, evidence also shows that treadmill exercise alone does not reverse foot-drop, which continues to impair gait and balance. This led us to develop and test ankle robotics as a means to improve ankle motor control.
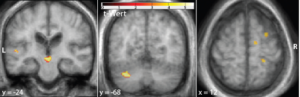 Evidence: Our initial randomized studies did not involve robotics at all. Instead, we studied treadmill training as a method to mediate locomotor learning while providing aerobic exercise as a cardiovascular health stimulus. Randomized clinical trials of 6 months progressive treadmill aerobic exercise training were compared to a control stretch program. Treadmill training improved walking function, even decades post-stroke, and improvements were linked with new activation of deep midbrain (panel 1) and cerebellar networks (panel 2), and peri-lesional cortex.
Evidence: Our initial randomized studies did not involve robotics at all. Instead, we studied treadmill training as a method to mediate locomotor learning while providing aerobic exercise as a cardiovascular health stimulus. Randomized clinical trials of 6 months progressive treadmill aerobic exercise training were compared to a control stretch program. Treadmill training improved walking function, even decades post-stroke, and improvements were linked with new activation of deep midbrain (panel 1) and cerebellar networks (panel 2), and peri-lesional cortex.
QUESTION #2: Can robotics mediate ankle motor learning after stroke?
Inspired by motor learning based upper extremity robot-aided rehabilitation for stroke and recognizing the critical role of the ankle in gait and balance, we collaborated with Newman Laboratory for Biomechanics and Human Rehabilitation at MIT to develop a modular, impedance-controlled ankle exoskeleton (Anklebot) as a laboratory research platform. This method of control and the embedded hardware assures safe and gentle interaction with frail humans. We investigated whether dorsi- and plantar flexion control of the paretic ankle could be improved using the Anklebot. We found that isolated, robot-aided ankle training while seated and in conjunction with a visually evoked task (video game) has been shown to improve key outcomes of ankle motor control in both early sub-acute and chronic phases of stroke and improve the speed and symmetry of unassisted walking. This proves that robotics can mediate motor learning across the paretic ankle during sub-acute and chronic stroke.
 Evidence: Seated ankle robot training in early sub-acute and chronic phases of stroke recovery were conducted for 6 weeks x 3 sessions/week. The robot parameters were personalized to each person’s deficit severity. During each session, the Anklebot applied “as-needed” assistance and measured the level of each person’s volitional ankle function. Subsequently, the protocol provided incremental challenge in both speed of movement and range of motion. We found that seated ankle robotics training improves the velocity, accuracy, and smoothness (reduced jerk) of ankle plantar (down) and dorsi-flexion (up) directions and improves symmetry of overground walking in persons with chronic hemiparetic stroke (6 months – 20 yrs. post-event). A separate randomized study at University of Maryland Orthopedics and Rehabilitation Institute (UMROI) found 2 weeks of seated ankle robotics effective to improve ankle motor control and symmetry of over-ground unassisted walking during early (<1 month) inpatient stroke rehabilitation.
Evidence: Seated ankle robot training in early sub-acute and chronic phases of stroke recovery were conducted for 6 weeks x 3 sessions/week. The robot parameters were personalized to each person’s deficit severity. During each session, the Anklebot applied “as-needed” assistance and measured the level of each person’s volitional ankle function. Subsequently, the protocol provided incremental challenge in both speed of movement and range of motion. We found that seated ankle robotics training improves the velocity, accuracy, and smoothness (reduced jerk) of ankle plantar (down) and dorsi-flexion (up) directions and improves symmetry of overground walking in persons with chronic hemiparetic stroke (6 months – 20 yrs. post-event). A separate randomized study at University of Maryland Orthopedics and Rehabilitation Institute (UMROI) found 2 weeks of seated ankle robotics effective to improve ankle motor control and symmetry of over-ground unassisted walking during early (<1 month) inpatient stroke rehabilitation.
QUESTION #3. Which motor learning model is most effective to improve gait and reduce foot drop after stroke
a) an impairment-based model that isolates ankle motor learning with seated computer video training, or b) a task-oriented training that integrates ankle robotics with treadmill walking?
Seated ankle robotics does not train the ankle in the context of walking. We did not assess potential to reverse foot drop. This led us to question whether ankle robotics could be more effective when combined with a locomotor learning task, such as treadmill walking, and to study effects on foot drop. In order to safely integrate ankle robotics with treadmill training, we embedded impedance control for “assist as needed” in an adaptive timing architecture that precisely times robotics assistance across any phase of the walking cycle. A randomized study in persons with chronic stroke compared 6 weeks x 3 sessions/week seated (videogame) versus treadmill + Anklebot on unassisted walking function and examined whether benefits are retained 6 weeks after completion of all training. The results of this study showed that “task-oriented” ankle robotics training was more effective than “impairment-based” isolated joint robotics training, and had potential to reverse foot-drop, restore safer and more efficient heel first foot landing, and reduce orthoses/assistive device needs.
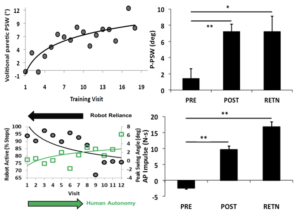 Evidence: Ankle robotics on treadmill, but not with seated training, restored ankle dorsiflexion during unassisted walking (top panel, P-PSW: paretic ankle swing), and these improvements were retained 6 weeks after completing all training. Treadmill based robotic training increased paretic ankle impulse indexing higher forward propulsion. These improvements coincided with a reduction in robotics reliance (human vs,rRobot contributions to ankle swing), revealing the time course of human-robotics cooperative learning toward autonomy. An unexpected finding was that many participants self-discarded their ankle braces and/or reduced assistive device needs. However, this study was limited by small sample size, and by the fact that treadmill training with a tethered and bulky, lab-based robot did not reflect a real world walking task to promote motor learning. This led us to design AMBLE as a lightweight, battery operated ankle robot, untethered for facile free-roaming as a tool in the hands of physical therapists.
Evidence: Ankle robotics on treadmill, but not with seated training, restored ankle dorsiflexion during unassisted walking (top panel, P-PSW: paretic ankle swing), and these improvements were retained 6 weeks after completing all training. Treadmill based robotic training increased paretic ankle impulse indexing higher forward propulsion. These improvements coincided with a reduction in robotics reliance (human vs,rRobot contributions to ankle swing), revealing the time course of human-robotics cooperative learning toward autonomy. An unexpected finding was that many participants self-discarded their ankle braces and/or reduced assistive device needs. However, this study was limited by small sample size, and by the fact that treadmill training with a tethered and bulky, lab-based robot did not reflect a real world walking task to promote motor learning. This led us to design AMBLE as a lightweight, battery operated ankle robot, untethered for facile free-roaming as a tool in the hands of physical therapists.
QUESTION #4: Can ankle robotics be used by therapists to reverse foot drop in the subacute stroke recovery period?
This is the question that we are now investigating in a randomized clinical trial. Our studies suggest that locomotor task-oriented training is an effective training modality, and human-robot contributions can be measured to quantify motor learning, and possibly manipulated by machine learning to optimize training in real-time. Thus, we ask whether untethered training with a wearable lighweight robot and machine learning to fine tune robotics assistance during real world physical therapy may provide the richest stimulus for recovery. We are now conducting a randomized, clinical trial in persons with subacute hemiparetic stroke (6 weeks to 6 months) and foot drop, to compare effects of robot (AMBLE) integrated physical therapy (9 weeks x 2/week =18 sessions) to physical therapy alone on outcomes of foot drop, assessed by clinicians blinded to treatment assignment), and biomechanics of unassisted over-ground walking. At the end of this study, we will be able to determine whether ankle robotics integrated into physical therapy during sub-acute stroke rehabilitation is more effective than best usual care, providing a new tool for therapists to address the foot drop impairment.
QUESTION #5: What are the Next Steps in robotics; how could this help improve function and health more broadly for persons with neurological disease?
NextStep Robotics is interested in receiving input from therapists, students, engineers, clinicians, and caregivers or persons with neurological conditions. As we launch our NIH-NINDS randomized clinical trial on ankle robotics to reverse foot drop after sub-acute stroke, we wish to expand our clinical, scientific, and consumer partnerships. Consider this an open source invitation toward our mission to innovate care, enablement, heart, and brain health for persons with diverse neurological disability conditions. NextStep scientific and engineering team can be reached at 443.869.3518.

